Hal Swerissen, La Trobe University
In a country like Australia, we all expect that when we get old, we’ll be able to rely on a robust aged care system. But aged care providers can’t find staff and a crisis is brewing.
If the problem isn’t fixed, there are serious risks to quality and access to services for older people who need support. There are also broader social, economic and political consequences for undervaluing the rapidly expanding health and social assistance workforce.
Aged care employs about 420,000 people. Around 80 per cent of those are front line staff providing care and demand for them is increasing rapidly.
Australians are ageing
The number of people aged 80 and over is projected to double by 2050. At the same time, informal family care is becoming less available. In the next 25 years, twice as many aged care staff will be needed.
Currently, about 1.4 million older people receive aged care services, including basic and more intensive home care and residential care.
Health care and social support job vacancies and ads are the highest of any industry. Between 30,000 and 35,000 additional direct aged care workers a year are already needed. By 2030 the shortfall is likely to be 110,000 full time equivalent workers.
Why don’t enough people want to work in aged care?
Despite recent pay increases, it is difficult to attract and retain aged care workers because the work is under-valued.
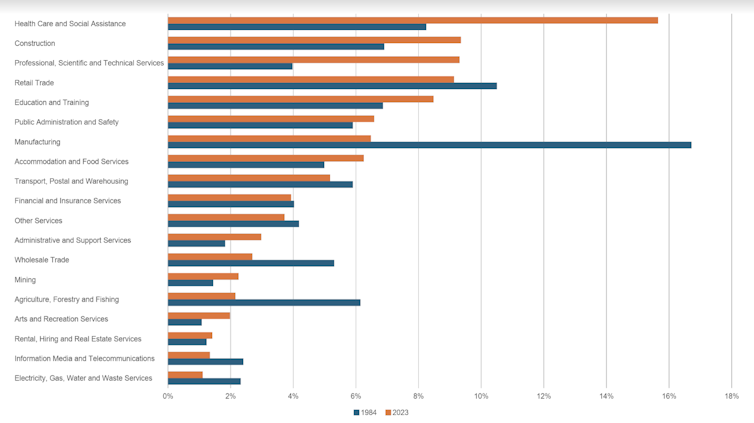
The Australian workforce is undergoing profound change. A generation ago, manufacturing made up 17 per cent of the workforce. Today it has fallen to 6 per cent. By contrast, the health care and social assistance workforce has doubled from 8 per cent to 16 per cent.
Manufacturing jobs were mainly secure, full-time, reasonably paid jobs dominated by male workers.
By contrast, jobs in aged care are often insecure, part-time and poorly paid, dominated by women, with many workers coming from non-English speaking backgrounds.
Since moving to take over aged care in the 1980s, the federal government has over-emphasised cost constraint through service privatisation, activity-based funding and competition, often under the cover of consumer choice.
The result is a highly fragmented and poorly coordinated aged care sector with almost 3200, often small and under-resourced providers centrally funded and regulated from Canberra.
This has led to high levels of casualisation, low investment in training and professional development, and inadequate supervision, particularly in the home care sector.
Aged care is facing a perfect storm. Demand for care and support staff is increasing dramatically. The sector is poorly coordinated and difficult to navigate. Pay and conditions remain poor and the workforce is relatively untrained. There are no minimum standards or registration requirements for many front-line aged care staff.
What are the consequences?
An understaffed and under-trained aged care workforce reduces access to services and the quality of care and support.
Aged care providers routinely report it is difficult to attract staff and they can’t meet the growing demand for services from older people.
Staff shortages are already having an impact on residential care occupancy rates falling, with some regional areas now down to only 50 per cent occupancy.

That means older people either don’t get care or they are at increased risk of neglect, malnutrition, avoidable hospital admissions and a poorer quality of life.
Inevitably, lack of aged care workers puts pressure on hospital services when older people have nowhere else to go.
What needs to be done?
Addressing these challenges requires a multifaceted approach. Australia will need a massive increase in the number of aged care workers and the quality of the care they provide. Wages have to be competitive to attract and retain staff.
But better pay and conditions is only part of the story. Unless aged care becomes a career the community recognises, values and supports, it will continue to be difficult to train, attract and retain staff.
The recent Royal Commission on Aged Care Quality and Safety highlighted the need for a more skilled workforce, emphasising the importance of ongoing professional development for all staff.
To date the federal government’s aged care workforce initiatives have been underwhelming. They are a limited and piecemeal rather than a coherent workforce strategy.
In the short term, skilled migration may be part of the solution. But progress to bring in skilled aged care workers has been glacial. Currently only about 1 per cent of providers have agreements to bring in staff from overseas. At best, overseas migration will meet only 10 per cent of the workforce shortfall.
Registration, qualifications and training for direct care work have to become mandatory to make sure care standards are met.
Much more significant and systematic incentives and support for training will be needed. Supervision, career progression and staff development will also have to be dramatically improved if we are to attract and retain the workforce that is needed.
“Learn and earn” incentives, including scholarships and traineeships for aged care, are needed to attract the future workforce.
At the same time, a much broader investment in upskilling the entire workforce through continuing professional development and good quality supervision is necessary.
Like manufacturing a generation ago, aged care needs to become valued, skilled, secure and well-paid employment if it is going to attract the staff that are needed to avoid a looming crisis.
Hal Swerissen, Emeritus Professor of Public Health, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
What do you think the solution to the staffing shortfall should be? Why not share your thoughts in the comments section below?


It all comes down to who wants to do the “dirty work”. The workplace & actual work can be depressing and the pay rates are nothing to write home about either.
Changing nappies on the elderly, cleaning up soiled bedding, treating bed sores, removing faeces from elderly patients bowels manually with your hand in a rubber glove simply doesn’t appeal to most.
You’ll find that some staff take it on until a better option comes along in another industry.
Unless staff are paid well to do those tasks , it’s going to be difficult to attract anyone while ever the unemployment rates are low.
You are so right in your summation of aged care.
“aged care needs to become valued, skilled, secure and well-paid employment if it is going to attract the staff that are needed to avoid a looming crisis” Absolutely correct.
Aged care was bad when my Mum was in a nursing home in the late 80’s. Because she was a “wanderer” (no security on doors back then) she was strapped to a chair for hours on end. It was depressing to visit and see her like that and even then the facility was understaffed.
Staff need to be well paid, respected and listened to by their Superiors.
Every time I read the Aged care providers crying poor my blood boils.
The expenditure priorities of eastern states providers with homes in Western Australia without serious discussion with residents And their families Leads to a waste of money..
senior management based in the East do not get it.