The science of fighting cancer has been taken to new levels, thanks to two independent research teams, one of which is in Australia. Each team has published an article in this month’s Nature revealing a breakthrough, which ‘supercharges’ bioengineered cancer-fighting cells.
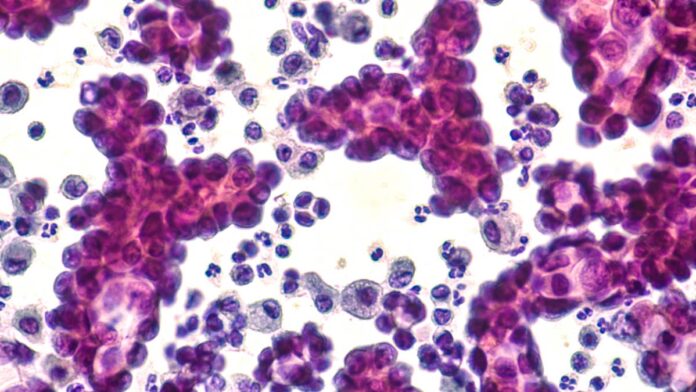
Bioengineered immune cells have been around for some time, and have been shown to effectively attack, and even cure cancer. However, those cells have also revealed a propensity to weaken over time, compromising their long-term effectiveness.
Separate teams working on immune cells known as CAR T cells have found that, if engineered to incorporate high levels of a certain protein, they are reinvigorated. Effectively, this makes them very much like stem cells, long known to have regenerative properties.
Aussies leading the way in cancer treatment
One of the teams that made the bioengineering breakthrough is based here in Australia, at Melbourne’s Peter MacCallum Cancer Centre. The other was a team led by immunologist Crystal Mackall at Stanford University in California.
Dr Mackell’s research team knew CAR T cells, made from immune cells called T cells, had a limited effective lifespan. The challenge then was to keep these CAR T cells active for longer, thus allowing them to eliminate cancers. This is especially important in the fight against solid tumours, such as those seen in lung and breast cancer.
Looking at previous CAR T treatments used on leukaemia patients, the team identified 41 genes that were linked to success. These genes appeared to be controlled by a ‘master-switch’ protein called FOXO1.
So Dr Mackell’s team engineered some CAR T cells to produce higher levels of FOXO1 than normal. These were injected into mice with various types of cancer and, bingo, the stem-cell-like cells shrank the mouse tumours more completely than earlier versions. Not only that, they also lasted longer in the body than standard CAR T cells did.
Great minds thinking alike
While all this was going on, the Peter MacCallum Cancer Centre team achieved the same results via a different method.
Led by immunologists Phillip Darcy, Junyun Lai and Paul Beavis, the team was examining an immune-signalling molecule called IL-15. The IL-15 molecule helped to switch T cells to a stem-like state but had one major drawback. The cells did not mature to the point where they fought cancer.
In searching for the cause of this ‘roadblock’, the team analysed CAR T cell gene activity. And lo and behold, they found that IL-15 turned on genes associated with FOXO1. Armed with this knowledge, Prof Darcy’s team mirrored the work of Dr Mackell’s team. They engineered CAR T cells to produce extra-high levels of FOXO1.
Their results were similarly promising. Not only did their supercharged cells become more stem-like, they also reached maturity and fought cancer without becoming exhausted.
“It’s the ideal situation,” said Prof Darcy.
Prof Darcy’s team also found an extra benefit of pumping up FOXO1 levels. They improved the CAR T cells’ metabolism, thus allowing them to last much longer when infused into mice.
This exceeded the team’s expectations. “We were surprised by the magnitude of the effect,” said Dr Beavis.
What next?
Dr Mackell said one of the most exciting aspects of the research was that FOXO1 worked the same way in mice and humans. “It means this is pretty fundamental,” she said.
It also paves the way for clinical human trials. Prof Darcy said his team was already speaking to clinical researchers about testing FOXO1 in CAR T cells. These trials could start within two years.
The research represents another step towards a cure for the beast that is cancer, one that kills around 50,000 Australians every year.
Have you or someone close to you been touched by cancer? Or do you know someone involved in cancer research? Let us know via the comments section below.
Also read: Aussies urged to boost cancer screening rates
Health disclaimer: This article contains general information about health issues and is not advice. For health advice, consult your medical practitioner.