Natasha Yates, Bond University
People aged 50 and over are now officially eligible to receive the AstraZeneca COVID-19 vaccine from selected GPs.
Although some practices have had permission to provide the vaccine early if they had excess stock, this marks a major step forward in Australia’s vaccination program.
People over 50 now have a choice of where to get vaccinated: their own GP (if taking part in the vaccination rollout), another GP practice (if their own GP is not), or respiratory clinics and mass vaccination hubs in some states.
Here are some practical things to think about when booking an appointment.
Can I speak to the GP first?
As a GP, I have been recommending patients access a vaccine from wherever is the most convenient for them. This may be from a mass vaccination hub or respiratory clinic, and not actually from a GP. However, some patients are hesitant and/or still have questions. If so, they do need to speak to a GP before they book for a vaccine.
The time to raise questions is not when you have turned up for your injection; most facilities allocate around 3-5 minutes for the doctor or nurse to spend with each patient. This does not allow time for prolonged discussion.
Instead, in the days before your vaccine, discuss concerns with your regular GP (if you have one). They know you and your medical history so are better placed to tailor advice to your individual situation.
If your GP is not one of the practices administering the vaccine, or if you don’t have a regular GP, you may want to book an appointment with a GP at the practice where you plan to get it, with the sole purpose of discussing your concerns.
Even if you book your vaccine through a GP clinic, it may not be a GP administering the vaccine. It may be a practice nurse, who is experienced at giving a range of vaccines and will have taken the same mandatory training as a GP in administering COVID-19 vaccines.
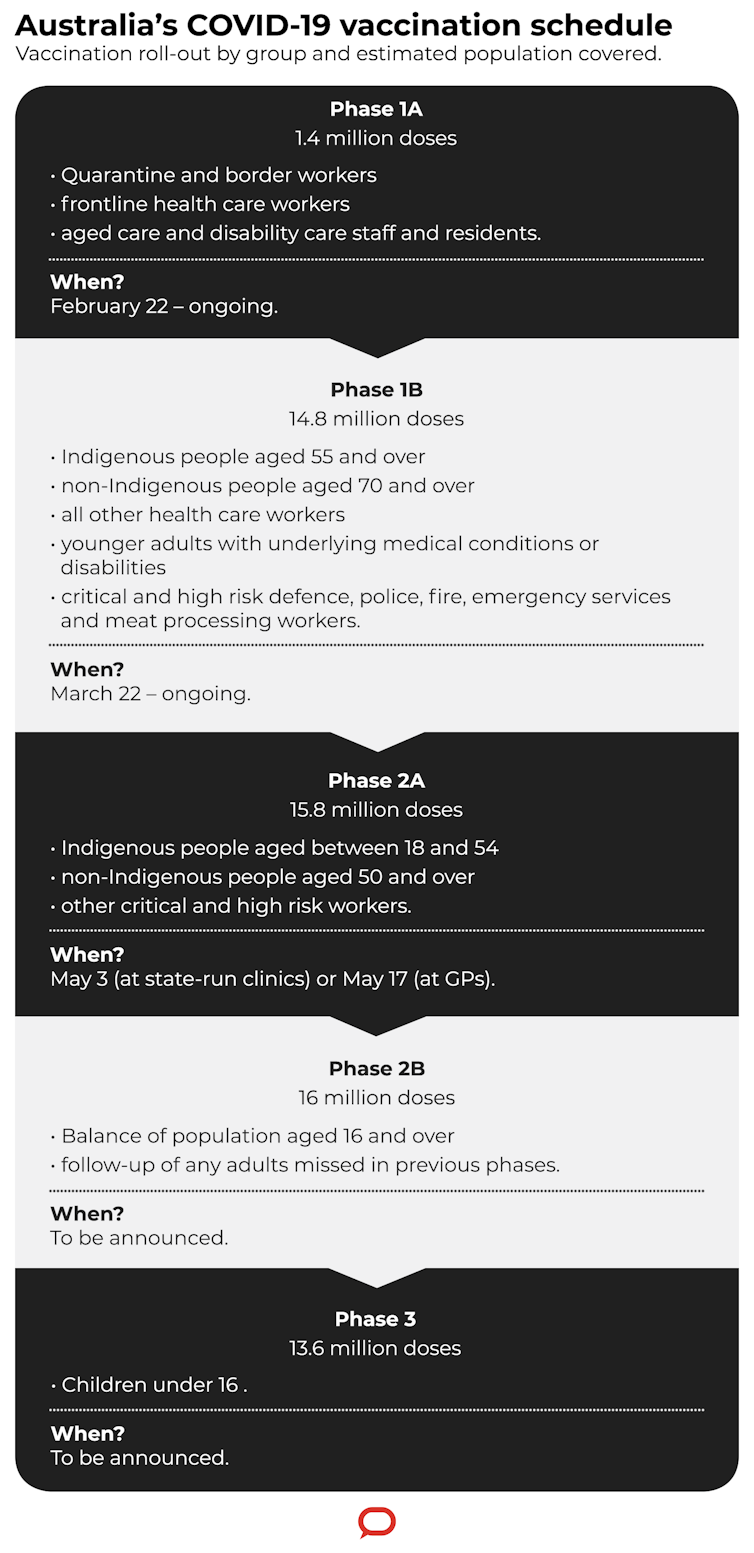
Department of Health/The Conversation, CC BY-ND
What’s the best time to have my vaccine?
The best time to get vaccinated against COVID-19 is as soon as possible, once you have had all your questions answered. However, there are a few things you may need to consider.
If you feel unwell
If you feel very unwell on the day, especially if you have a high fever (over 38 degrees C), you need to postpone your vaccine. This is partly because your immune system may not respond optimally to the vaccine, and partly so symptoms after the vaccine aren’t confused with symptoms from an underlying illness.
If you want the flu vaccine too
It’s best to leave at least 14 days between your influenza and COVID-19 vaccines. It’s likely safe to have them both together, however this is still being tested. Also, if you happen to get a reaction to one of them, you will know which one you have reacted to.
If it’s time for your mammogram
As the vaccine can cause a temporary swelling of the lymph nodes in the armpit, women are advised to either have a mammogram first, or delay it until six weeks after vaccination. This advice is particularly relevant as we start to vaccinate women 50 and over, the key target group for Australia’s breast cancer screening program.
If you can, book before a scheduled day off
About 20% of people report missing work, study or routine duties for a short period after their first AstraZeneca vaccine. So have your vaccine the day before a scheduled day off work if possible.
Should I take a painkiller directly before or after my vaccine?
Unless you take common painkillers such as paracetamol, ibuprofen or aspirin regularly to treat an underlying illness, do not take medications that control pain and/or fevers before your vaccine.
You may use them after the shot but only if you need to treat symptoms that are worrying you. Overall it is best to avoid taking them at all as they may curb your immune response.

from www.shutterstock.com
Both paracetamol and ibuprofen can reduce the immune response to other vaccines, particularly in children, although we’re not certain how much this affects their overall immunity to that disease.
One study showed taking aspirin, paracetamol or ibuprofen resulted in suppression of part of our immune response to viruses. And another study, this time in mice, revealed anti-inflammatory medications can impair production of some immune molecules after COVID-19 infection.
While none of this is strong evidence against taking these medications around a COVID-19 vaccine, the take-home message is not to take them if you don’t need to.
What about exercise before and after the vaccine?
Being physically fit can help you fight off upper respiratory tract infections. However, does that translate to exercise also helping your immune response to vaccines? In other words, if you exercise before or after a vaccination will it work better?
There is evidence exercise can help improve the response to some vaccines, particularly the influenza ones, but this does not apply to all vaccines.
While the jury is still out on whether your COVID-19 vaccine will work better if you exercise around the time of having it, here is my suggestion: don’t exercise more than you usually do in the days before or after your shot.
Muscle pain and fatigue are two of the commonest side-effects from the COVID-19 vaccine, and are also normal responses to increasing your exercise. Avoid complicating the picture by maintaining your usual fitness regimen, and give yourself some leeway in the days after the vaccination where you may be feeling the side-effects from it.
The US Centers for Disease Control recommends using or exercising your arm after the shot to help reduce pain and discomfort (although not to help the vaccine work better).
Use the government’s vaccine eligibility checker to see if you’re next in line for the COVID-19 vaccine, and where you can get vaccinated.![]()
Natasha Yates, Assistant Professor, General Practice, Bond University
This article is republished from The Conversation under a Creative Commons licence. Read the original article.
Will you be getting your vaccine shot from a GP? Is your local GP offering COVID-19 vaccinations?
If you enjoy our content, don’t keep it to yourself. Share our free eNews with your friends and encourage them to sign up.

