A new medical device to reduce the risk of complications following a common procedure to unblock clogged arteries is being developed by Monash University researchers.
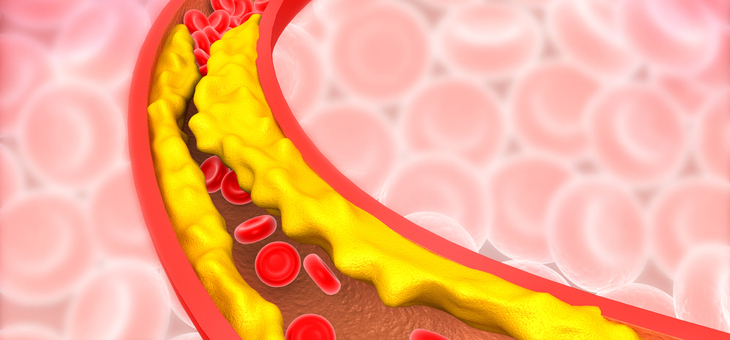
Narrowing of the arteries, called atherosclerosis, is the most common cardiovascular disease and affects hundreds of thousands of Australians and millions around the world.
Plaque builds up inside the arteries that carry oxygen-rich blood around the body and, over time, hardens and narrows the arteries. This limits the flow of oxygen-rich blood to organs and other parts of the body and can lead to heart attack, stroke and even death.
A current treatment, balloon angioplasty, involves inflating a small balloon in the affected area of the artery to increase blood flow. Coating the balloon with a drug that prevents re-narrowing of the vessel has been added to the procedure.
However, recent studies have found that paclitaxel – the drug used to coat the balloon – may cause serious side-effects, including toxicity around the region of the balloon, up to two years after the procedure, prompting the US Food and Drug Administration (FDA) to issue a medical device safety communication.
The Eastern Health Clinical School at Monash University is now developing an alternative treatment that uses a light-activated drug to coat the angioplasty balloon and reduce the risk of toxicity.
Associate Professor Anthony Dear said the device, called Lumi-Solve, ensured the drug was targeted to the site of the narrowed artery, and was activated only when exposed to UV light.
“Under the existing angioplasty procedure, when you open a balloon that’s coated with a drug, a lot of it showers off and travels into the blood vessel down the leg, potentially causing reactions away from the intended area,” Assoc. Prof. Dear said.
“With our system, the drug is not active until the balloon is open and touching the vessel wall at the affected site and then exposed to light, potentially significantly reducing local and systemic toxicity.
“Tens of thousands of people undergo a balloon angioplasty each year, so the benefits of this new technique are potentially enormous.”
Assoc. Prof. Dear said the procedure might also be safer than treating clogged arteries with stents, as they can cause ongoing health problems.
“As stents are permanent ‘foreign bodies’, they may cause blood clots, which requires patients to take life-long blood thinners,” he said.
“And because stents are not flexible, they can fracture and rupture the artery wall in some areas of the body, particularly where they cross joints such as hips and knees.”
Assoc. Prof. Dear said researchers had been working on the new device for several years – well before the FDA communication – and involved scientists from a number of institutes including the Bio21 Institute at the University of Melbourne, the CSIRO and Baker IDI.
He said the study in the Lumi-Solve development program, which was supported by funds from Monash University and the NHMRC, focused on treating narrowing in leg arteries, but that the new procedure could easily be applied to other areas of the body, including coronary and neck arteries.
They are now working on further development and evaluation of the device.
Were you aware of the dangers of the drug used to coat the balloon?
If you enjoy our content, don’t keep it to yourself. Share our free eNews with your friends and encourage them to sign up.
Related articles:
How flying affects your body
Drugs, drink affecting more seniors
A better shot at staying independent