The nation’s GPs say the health sector is in crisis, urgently needs properly funded reform and that some aspects of Medicare should be revamped.
At the same time, surgeons say privately insured patients are being discriminated against with public patients getting priority in the private system because of government pressure.
The Royal Australian College of General Practitioners (RACGP) says doctors are buckling under the pressure of COVID demands and believe that will only escalate as restrictions ease and COVID infections spike.
The RACGP’s General Practice: Health of the Nation report – an annual health check-up on general practice – paints a sombre picture.
Read: Vaccine boosters available within weeks
RACGP president Dr Karen Price says general practice must be resourced properly to manage the long-term fallout from the pandemic and to take pressure off emergency departments and hospitals.
“For the next two years, GPs will manage fully vaccinated people with mild cases of COVID-19, the rollout of booster shots and the huge backlog of care from lockdown, which will mean a need for more hours, funding and staff,” she says.
In the week ending 2 October, one in 10 new COVID cases in NSW had been double- vaccinated – an indication of the added pressure set to be placed on GPs.
The college says changes must be made to Medicare items, particularly in relation to mental health conditions.
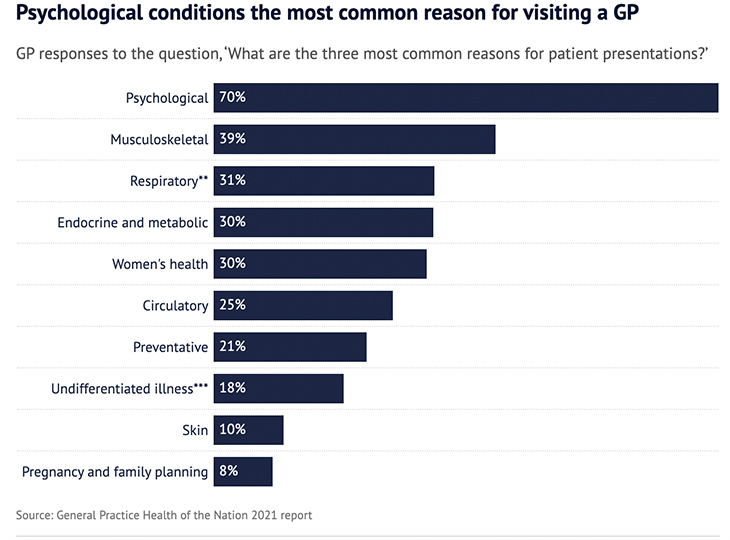
“We know that more and more patients are presenting with mental health concerns,” Dr Price said. “Our survey found that for the fifth consecutive year, psychological conditions were the most reported reasons for patient presentations.”
She says that to help those patients, new Medicare items for longer mental health consultations were desperately needed so GPs could “really get to the bottom of what is going on”.
The college is also critical of other aspects of Medicare.
Dr Price says that GPs are the only medical practitioners who specialise in managing patients with multiple health conditions, “yet Medicare discourages GPs from treating more than one condition in the same consultation”.
This must change, she says. “Now more than ever, it is essential that we remove this barrier and incentivise longer consultations to support comprehensive care by GPs.”
The report found that the proportion of GPs who bulk-bill rose to 89 per cent in 2020-21, up from 86.2 per cent in 2018-2019, and that the average out-of-pocket cost for a consultation was $41.12, an increase from $27.65 in 2012.
Read: Ambulance ramping a symptom of health system in distress
The long-term effects of the pandemic on elective surgery waitlists are only now starting to be felt.
Lloyd Adams, executive manager of Health Care Australia, said that some surgery waitlists, including hip and knee replacement surgery, were already two to three years in some areas.
“The latest COVID-19 outbreak has further impacted these waitlists, with thousands of surgeries delayed and patients having to continue living with immobility and debilitating pain, not knowing when they will be able to have the surgery done,” he said.
And, bizarrely, public patients in Victoria are being prioritised ahead of private patients.
A group of Melbourne surgeons says privately insured patients are being pushed to the back of the queue under a state government deal to prioritise public patients for elective surgery in the private system, The Age reports.
Read: Why your blood pressure changes with age
Vascular surgeon Susan Morris says her private patients are having their surgery cancelled “indefinitely” even though some are in severe pain.
She estimates she is cancelling non-urgent elective surgery for 75 per cent of her private patients and that her surgical lists are instead full of public patients, who have been on a waiting list for three years.
“It is not as if surgeons are not wanting to help the public sector, but it shouldn’t be a complete punishment if you’re a privately insured patient,” she says.
“What the government has done is move the problem from the public sector to the private sector. Some of these privately insured patients are more severe cases but they are getting pushed to the back of the line. It is not morally right.”
Would you like to see changes to Medicare? Have you been waiting for elective surgery? Why not share your experience in the comments section below?
If you enjoy our content, don’t keep it to yourself. Share our free eNews with your friends and encourage them to sign up.

