In case you missed it, perimenopause is in the news.
It came about as a result of Pursuit’s editor Imogen Crump experiencing a perimenopausal hot flush live on ABC News Breakfast television while talking about the big news stories of the day with hosts Lisa Millar and Michael Rowland.
Instead of pretending it wasn’t happening – Imogen owned it. And that has started a national conversation.
Do I wish I hadn’t had a #perimenopause #hotflush on live TV? Yes. But if it’s a step toward having public conversations about something that at least half the population will experience in some form or other, then good. @abcnews pic.twitter.com/jw6v5GJlHd
— Imogen Crump (@ImogenJC) November 9, 2023
“I’m so sorry, I could keep stumbling through, but I’m having such a perimenopausal hot flush right now, live on air, sorry,” Imogen said to the hosts, while fanning herself with her notes.
“I don’t think hormones respect national television.”
Lisa Millar stepped in. “We need to make it normal to have these kinds of conversations and I love you for even saying it, because we interview people, we talk to people about this and this is the reality.”
But is it weird that in 2023 perimenopause should still be so taboo that a woman having a hot flush on TV is a big deal?
Perimenopause is not a secret. All women go through it in some form or another. In fact, around 32 per cent of women in Australia are currently experiencing symptoms they attribute to menopause, which can severely affect the day-to-day life of at least one quarter of Australian women aged between 45 and 64.
So what do you need to know about perimenopause? Here are five simple answers to five basic questions to help demystify something that’s entirely normal.
Q. What’s the difference between perimenopause, menopause and postmenopause?
Menopause refers to a women’s final menstrual period. Natural menopause usually occurs between the ages of 45 and 55 years old, which marks the end of your reproductive age. You are considered postmenopausal if you’ve had no period at all for 12 months.

Perimenopause happens before menopause. It starts when menstrual cycles become very irregular (so the length of your cycle can vary by seven or more days in consecutive cycles) and continues until 12 months after you’ve had your final period. For some, perimenopause can begin five to 10 years before their final period.
But you can just use the term menopause as it’s divided into those three basic stages: perimenopause, menopause and postmenopause.
There are also other variables here – like surgical or treatment-induced menopause, early menopause (which can happen between the ages of 40 and 45) or premature menopause (which can occur below the age of 40).
Q. What’s actually happening and why?
Essentially, perimenopause, menopause and postmenopause are terms that all refer to the effect of declining circulating oestrogen (a group of hormones that play an important role in the normal sexual and reproductive development in women) in your body.
At birth, ovaries contain a certain number of cells (called follicles) which are involved in every menstrual cycle over a woman’s reproductive life.
As these follicles age and the number of follicles decline, there is a resulting impact on function and, consequently, circulating blood oestrogen levels drop. Menopause occurs because of this decline.

Perimenopause, which includes the menopause transition, is typically characterised by fluctuating hormones and irregular cycles (shorter or longer).
And this is when you’ll start to experience typical (and occasionally weird) menopausal symptoms.
Q. Let’s talk symptoms, what can women expect?
There are so many perimenopausal symptoms linked to either an excess or loss of oestrogen. Women can experience both extremes as their hormones fluctuate.
Symptoms associated with excess oestrogen include heavy menstrual bleeding, sore breasts and headaches.
A recent global initiative has identified the symptoms associated with a loss of oestrogen – and it’s a long list.
It includes hot flushes and night sweats (known as vasomotor symptoms), sleep disturbances, and symptoms related to vaginal dryness (or genitourinary symptoms) – like vulval or urinary discomfort.
Other symptoms include mood changes, fatigue, cognitive concerns and a low libido, as well as joint and muscle pain or stiffness.
Another important consideration is that declining oestrogen also has implications for chronic disease risks. In particular, bone loss and heart health.

As our hormones bounce around, it can increase our osteoporotic and cardiovascular risk, which is associated with metabolism and body composition changes. There may also be increased risk of mood disorders for those who have a history of hormone-related issues.
And, to top it off, our cancer risk may also change – so making sure you’re up-to-date with bowel, breast and cervical cancer screening is very important.
Q. Then there’s mental wellbeing
The menopause transition phase can be a time where your mood and cognition are impacted – even in people with no prior history of mental health concerns.
And these mood changes can be quite unique and variable.
Some women report irritability or paranoia, while others experience increased anger, and then there are the women who report feeling less sad. Or it could be all of these at once.
These mood changes can last for varying amounts of time (from minutes to hours) and then just as suddenly, stop.
It does appear that the more physical symptoms (like vasomotor symptoms) or negative life events you have during this very changeable time can increase your risk of depressive symptoms. There is also a higher risk of a major depressive episode associated with perimenopause (compared with before your body starts to transition).

Then there are the cognitive changes. Around two-thirds of women report memory problems or reduced processing speed during perimenopause – known by many as ‘brain fog’.
While we haven’t found a direct link between mood or cognition and menopause, oestrogen has been associated with changes in the brain. Hot flushes are also linked to changes in brain function and depression can be associated with cognitive decline.
The good news here is that most mood and cognition changes are thought to be temporary and do not continue in the postmenopausal period.
Q. What about treatment? What are the options?
If symptoms are interfering with your daily life – seek medical advice.
The current gold standard treatment for vasomotor symptoms is Menopausal Hormonal Therapy (MHT), formerly known as Hormone Replacement Therapy (HRT).
The idea of MHT is that it replaces the hormones that are naturally produced in your body with the aim of improving hot flushes and night sweats for 80 to 90 per cent of women.
The Australian Menopause Society (AMS) recommends that MHT is offered if symptoms are really bothering you or impacting on your quality of life. For more on the different types of MHT, head to the AMS website or Health Direct.
It is important here to discuss concerns about the link between MHT and breast cancer.
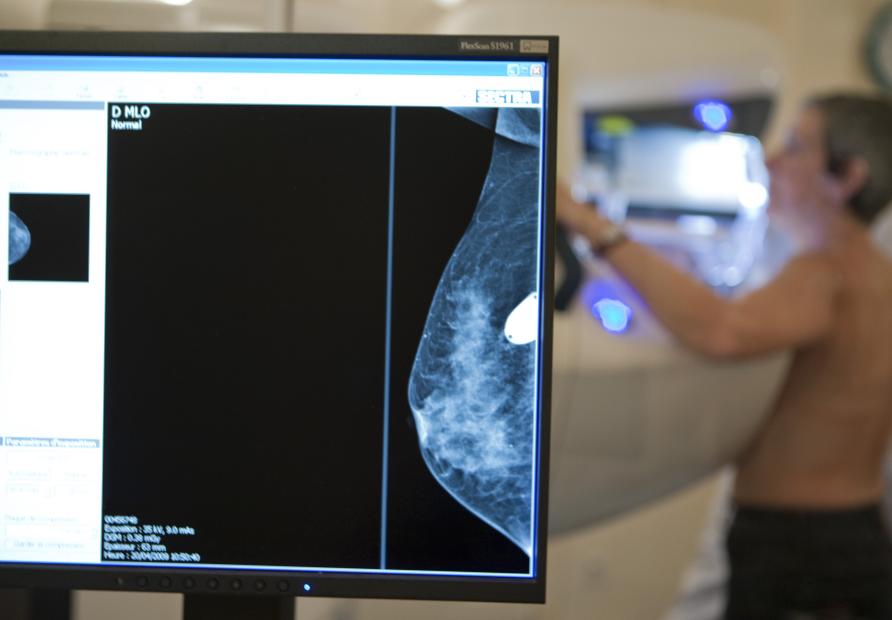
The British Menopause Society, the International Menopause Society, the European Menopause and Andropause Society, the Royal College of Obstetricians and Gynaecologists and the Australasian Menopause Society released a joint statement on MHT and breast cancer risk in 2020 which highlighted the small risk that appears to be dependent on the type of MHT.
In fact, findings from the recent Women’s Health Initiative placebo-controlled randomised trials show a decrease in the risk of breast cancer with oestrogen-only MHT. Other research reports that micronised progesterone is a lower risk option.
The bottom line is to talk with your doctor about the risks and benefits and then make an informed choice.
However, not everyone needs, wants, or is able to use MHT.
Non-hormonal treatments can include certain antidepressants, an anticonvulsant, and a blood pressure medication that helps hot flush reduction.
Many women also benefit from lifestyle changes like improving diet and regular exercise, stopping smoking, dressing in layers, avoiding spicy food, avoiding excess alcohol and caffeine and looking at therapies like Cognitive Behavioural Therapy (CBT). While these won’t necessarily reduce symptoms, they can make it easier to cope with the symptoms.
Hot flushes aren’t the only symptom that may need treatment. There are a number of treatments out there that can help you to manage heavy menstrual bleeding, genitourinary issues, sleep disturbances and joint pain.

The important message here is that if symptoms are really affecting you, get medical advice because there are options available to you.
That all said, the more we talk about perimenopause, menopause, and postmenopause, the more we educate the people around us. It’s not a mystery or a secret – just something most women experience and they should be encouraged and supported as they make their (occasionally sweaty) way through it.
Did you suffer during perimenopause? Did you do anything to treat it? Why not share your experience in the comments section below?
Also read: What you need to know about depression during menopause

This is all good information however not all things are as they seem. I have been post menopausal since my mid 40s following a hysterectomy. I was placed on HRT and continued for 35 years when I developed breast cancer. My HRT was discontinued immediately and I went into surgery. All went well there, however 7 years later at 85years of age I am still dealing with hot flushes and have yet to find a way to reduce them despite several different medications. So as wonderful as the HRT was and the great benefits of it, if only the medical people who prescribed it to me had advised to slowly decrease the dosage as I aged it maybe would have been helpful and I would not be finding life so difficult now. Post breast cancer I cannot resume it.